
It is not legal advice, nor is it advice about how to code, complete or submit any particular claim for payment.
CPT CODE FOR POST VOID BLADDER SCAN FULL
The code and full description are as follows:ħ6857 Ultrasound, pelvic (nonobstetric), real time with image documentation limited or follow-up (eg, for follicles)ĭisclaimers The information provided is general reimbursement information for Bracco products. “When a bladder-only study (male or female) with and without post-void residual is ordered and performed, code 76857, Ultrasound, pelvic (nonobstetric), real time with image documentation limited or follow-up (eg, for follicles), should be reported” ( Clinical Examples in Radiology Volume 9, Issue 3 Summer 2013). Code 51798 should only be reported if a bladder volume study or post-void residual measurement is obtained without imaging.Īnd Clinical Examples in Radiology, co-published by the AMA and ACR included the following in a test case discussion: Guidelines in the CPT book tell us code 76857 should be reported for a bladder ultrasound. The correct CPT code for a bladder pre- and post-void with ultrasound would be limited pelvis, CPT code 76857.
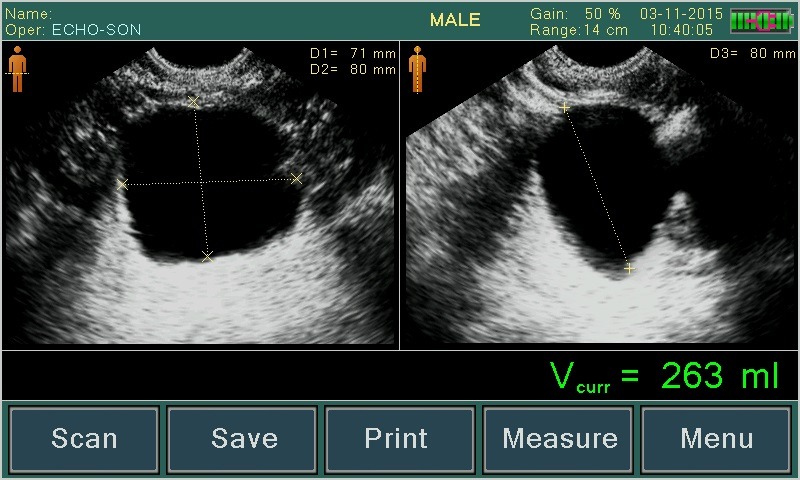
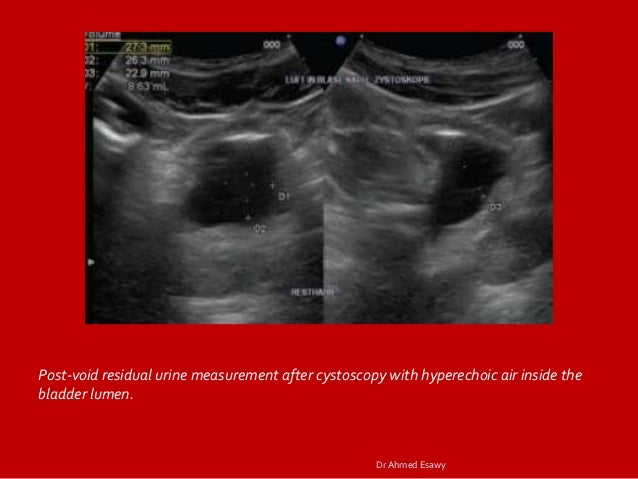
Be aware that there may be a mild burning sensation during the first void.Inform the nurse of the void so that the amount can be measured and documented. Void when able with the goal to urinate within six hours after removal of the catheter.Increase or maintain fluid intake (unless contraindicated).When a urinary catheter is removed, instruct the patient on the following guidelines: If a bladder scanner is not available, a straight urinary catheterization is performed.A bladder scan is a bedside test performed by nurses that uses ultrasonic waves to determine the amount of fluid in the bladder. If urination volume is less than 180 mL, the nurse should perform a bladder scan to determine the post-void residual.The patient should be prompted to urinate.The ANA has made the following recommendations to assess for incomplete bladder emptying: If the patient is unable to void within 4-6 hours and/or complains of bladder fullness, the nurse determines if incomplete bladder emptying is occurring according to agency policy. This information is also communicated during handoff reports. When removing an indwelling urinary catheter, it is considered a standard of practice to document the time and track the time of the first void. For additional instructions about how to remove an indwelling catheter, see the “ Checklist for Foley Removal.” Some agencies have a protocol for the removal of indwelling catheters, whereas others require a prescription from a provider. For patients who require an indwelling catheter for operative purposes, the catheter is typically removed within 24 hours or less. Prolonged use of indwelling catheters increases the risk of developing CAUTIs. It is the nurse’s responsibility to assess for a patient’s continued need for an indwelling catheter daily and to advocate for removal when appropriate.


 0 kommentar(er)
0 kommentar(er)
